Epidemiology
Prevalence is estimated at around 1 in 30,000 males. Hemophilia primarily affects males, but a symptomatic form of hemophilia B in female carriers has also been described with a generally milder clinical picture.
Clinical description
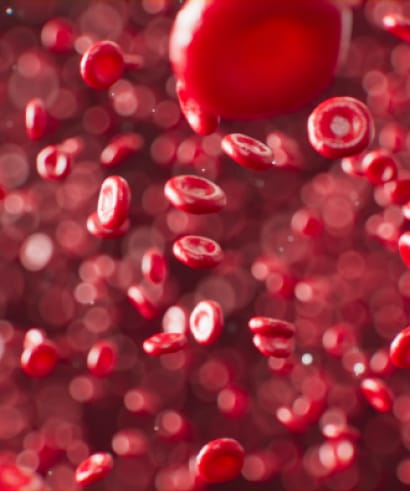
In general, onset of the bleeding anomalies occurs when affected infants start to learn to walk. However, newborns with hemophilia are at risk of intra- or extracranial hemorrhage and other bleeding complications. The severity of the clinical manifestations depends on the extent of the factor IX deficiency, both in males and in females. If the biological activity of factor IX is below 1 IU/dL, hemophilia is severe and manifests as frequent spontaneous hemorrhage and abnormal bleeding as a result of minor injuries or following trauma, surgery or tooth extraction (severe hemophilia B). If the biological activity of factor IX is between 1 and 5 IU/dL, hemophilia is moderately severe with abnormal bleeding as a result of minor injuries or following trauma, surgery or tooth extraction but spontaneous hemorrhage is rare (moderately severe hemophilia B). If the biological activity of factor IX is between 5 and 40 IU/dL, hemophilia is mild with abnormal bleeding as a result of minor injuries or following trauma, surgery or tooth extraction but spontaneous hemorrhage does not occur (mild hemophilia B). Bleeding most often occurs in joints (hemarthroses) and muscles (hematomas), but any site may be involved following trauma or injury. Spontaneous hematuria is a frequent and highly characteristic sign of the disorder.
Etiology
Hemophilia B is caused by mutations in the F9 gene (Xq27) encoding coagulation factor IX.
Diagnostic methods
Diagnosis is suspected on the basis of coagulation tests revealing prolonged blood coagulation times (activated partial thromboplastin time – aPTT) and can be confirmed by specific measurements of factor IX activity and antigen levels.
Differential diagnosis
The differential diagnosis should include hemophilia A, von Willebrand disease, and other coagulation anomalies leading to prolonged blood coagulation times.
Antenatal diagnosis
Prenatal diagnosis performed on chorionic villi or amniocytes is rapid and informative when the familial, causative F9 mutation is known. Knowing the familial F9 mutation status in the fetus allows for preparation of delivery and early newborn medical management.
Genetic counseling
Inheritance is X-linked recessive and genetic counseling is recommended for affected families. For a female carrier, there is a 50% risk that male offspring will be affected and a 50% risk that each female offspring will be carriers. Female carriers may express mild to moderate symptoms. Overall, there is a 25% risk for each pregnancy that the baby will be a male offspring with hemophilia and a 25% risk that the baby will be a heterozygous female offspring.
Management and treatment
Treatment is provided by multidisciplinary comprehensive hemophilia care centers. Replacement therapy consisting of administration of the missing factor IX (plasma-derived or recombinant factor IX concentrates) is the usual treatment approach. Recently, bioengineered prolonged half-life factor IX products were approved for the treatment of hemophilia B and significantly improve the quality of life of patients. Treatment may be administered after a hemorrhage (treatment on demand) or to prevent bleeding (prophylactic treatment). The most serious complications are production of inhibitory antibodies against the administered coagulation factor and anaphylactic shock in response to factor IX therapy. Surgical interventions, most notably orthopedic surgery, may be carried out but should be conducted in specialized centers.
Prognosis
Left untreated, the disease course is severe and in, severe hemophilia B, is generally fatal. Insufficient or incorrect treatment of recurrent hemarthroses and hematomas leads to physical impairment with severe disability associated with stiffness, joint deformation and physical disability. However, current treatment approaches (early prophylaxis) prevent these complications and the prognosis is favorable. Hemorrhage, HIV and HCV infections, and hepatic disease are the leading causes of death in patients with hemophilia.